
Born on April 25, 1989, in Boxtel, Netherlands, professional darts player Michael van Gerwen is a professional athlete with millions of fans. Those who did not recognize him with his bright green shirt heard his name in 2023 when he came up with another issue and started to follow him on social media. He explained his health problem to the press, stating that health is more important than anything else.
Michael van Gerwen, who started his darts career at the age of 13, became world champion in 2014, 2017, and 2019, winning the PDC (Professional Darts Corporation). His skills and determination took him to the top of his career. Now he is using that same determination to solve his health problem. “They're going to move my upper jaw forward six millimeters and put my lower jaw back only three millimeters,” he told the press, explaining that he has difficulty eating properly due to his prominent underbite.
His friend Vincent van der Voot described Michael van Gerwen health problem as follows: "He was very quiet. Michael van Gerwen's teeth are crooked, he has eight millimeters gap between his front teeth. It looks really strange. He's ashamed of it. He doesn't feel comfortable with the situation. He remained silent throughout the match. We all hope it will be back to normal soon. However, the resolution of this issue won't occur within a few days".
What was Michael van Gerwen's disease? What did the condition he mentioned in his statement mean? Michael van Gerwen suffered from underbite (prognathism), a condition in which the lower jaw is positioned in front of the upper jaw, and a class 3 malocclusion. That is, Michael Van Gerwen's upper jaw was smaller than his lower jaw, and his lower jaw was abnormally protruding forward. This affected his biting, breathing, and sleep, as well as causing headaches. Therefore, he underwent extensive dental and jaw surgery in 2023. During the operation, both her upper and lower jaws were repositioned, and then she was treated with braces and is recovering well.
Now, let's examine in detail the underbite (prognathism) problem experienced by Michael van Gerwen and its solutions.
What is prognathism?
Prognathism is the outward extension or protrusion of the lower or upper jaw. In other words, one of the lower or upper jaws is protruding forward. This results in the positioning of the upper or lower teeth in front.
The effects of prognathism can be mild or severe. Some cases are more pronounced than others and can significantly affect quality of life. In addition to pain and chewing problems, it can give a person an angry or belligerent appearance.
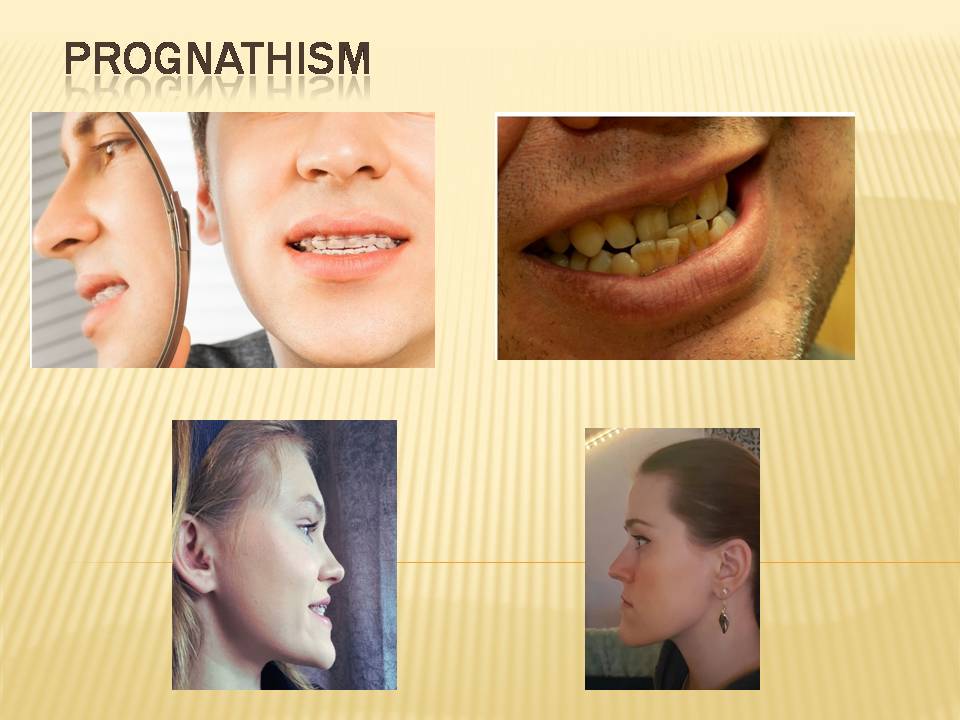
Types of prognathism:
There are three types of prognathism:
Mandibular Prognathism:
This is a condition in which the lower mandible (mandible) is protruded forward relative to the upper jaw (maxilla). This causes the lower teeth to be positioned in front of the upper teeth. It is the most common type.
Maxillary prognathism:
It is a condition in which the upper jaw is positioned forward . Also known as alveolar prognathism.
Bimaxillary prognathism:
A condition in which both the upper and lower jaw are protruding outward
Causes of prognathism:
Genetic factors causing the developmental problem in the jaw structure:
Prognathism is largely genetic. This implies that parents directly pass it on to their children without any underlying medical conditions. There may be many syndromes underlying developmental disorders of the jaw structure, or developmental disorders of the jaw structure may be the harbinger of many syndromes. These include:
Acromegaly:
This disease, which occurs when the pituitary gland secretes too much growth hormone, causes excessive growth and enlargement of organs such as hands, feet, and the face. This disease can lead to enlarged tissues, such as an oversized chin.
Crouzon syndrome:
Crouzon syndrome is a condition in which some of the bones in the baby's skull fuse too early, preventing the skull from growing properly. This syndrome is rare. In Crouzon syndrome, the area of facial bones between the eyes and upper jaw is small. This can cause the lower jaw to protrude forward. A genetic mutation causes Crouzon syndrome.
Basal cell nevus syndrome:
Basal cell nevus syndrome refers to a group of irregularities of the skin, endocrine nervous system, eyes, and bones caused by a rare genetic condition. It is an inherited syndrome that includes tumors and cysts of the skin, odontogenic keratocystic tumors of the jaw bones, cleft lip and palate, calcifications of the meninges, pits on the palms and soles, various tumors, mesangial cysts, and bone formations. This inherited condition causes abnormal facial development.
Acrodysostosis:
This genetic disorder has a negative impact on bone growth. Symptoms include short arms and legs, an abnormally shaped head, a short nose, and an oddly small jaw and mouth. There is usually a small upper jaw, which makes it appear larger compared to the lower jaw.
Down syndrome (mongolism),
An extra chromosome in the 21st chromosome pair causes Down syndrome, a genetic condition. This extra chromosome can cause physical growth retardation, moderate mental retardation, and, in some cases, excessive chin growth.
Dental malocclusions:
Misalignment of the upper and lower teeth (malocclusion) can affect the position of the jaw, leading to the development of prognathism.
Childhood habits:
Parafunctional oral habits such as finger sucking, tongue thrusting, thumb and pacifier sucking, prolonged bottle feeding, and nail biting may also occur later in life.
Overuse of pressure on the jaw muscles
Voluntary or involuntary habits such as teeth grinding and clenching can cause changes in the jaw structure.
Traumas:
Jaw traumas in childhood or adolescence can cause prognathism by disrupting the normal growth and development of the jaw bones.
Symptoms of prognathism:
Common prognosis signs include:
- Dislocated jaw (dislocation of one or both upper or lower jaws)
- Temporomandibular joint (TMJ) disorders.
- Tooth erosion.
- Bruxism.
- Overbite or underbite.
- Tooth misalignment.
- Difficulty chewing.
- Speech problems.
- Shortness of breath.
If you have one or more of the symptoms listed above, you should consult a doctor immediately. The doctor will refer you to the necessary specialists for the resolution of your problem(s).
What exactly was Michael van Gerwen's health problem, and what symptoms did he have?

Michael van Gerwen had mandibular prognathism and Class 3 malocclusion problems. Before explaining these problems and treatment methods, let us briefly summarise these two definitions.
Mandibular prognathism:
Michael van Gerwen's lower jaw was positioned anteriorly compared to his upper jaw. This is called mandibular prognathism.
Michael van Gerwen's mandibular prognathism caused him breathing and sleeping problems as well as headaches.
Class 3 malocclusion:
The misalignment and improper fit of Michael van Gerwen's upper and lower teeth limited his ability to chew and speak. This condition is called a Class 3 malocclusion. In a Class 3 malocclusion, the lower teeth are too far forward compared to the upper teeth and are usually the most difficult type to correct.
What is Mandibular prognathism?
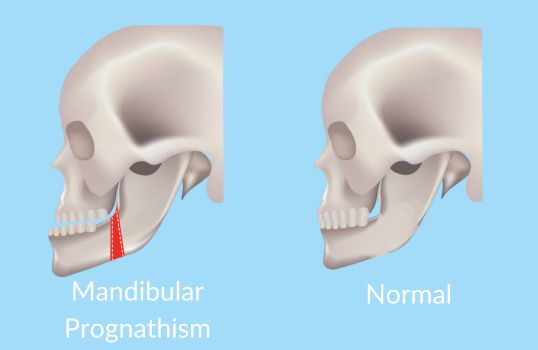
Mandibular prognathism, as described above, is a condition in which the lower jaw (mandible) is abnormally protruding forward more than the upper jaw. A jaw disorder known as "class III malocclusion" typically arises from mandibular prognathism.
What problems does mandibular prognathism cause?
Headaches and sleep problems:
When the upper jaw is too small, the nose receives less oxygen, leading to issues like headaches and reduced sleep. It can also cause sleep apnoea.
Inadequate bite:
Difficulty chewing due to teeth not closing properly will cause an inadequate bite. Inadequate bite can cause other problems, such as bad breath, digestive problems, and temporomandibular joint disorders.
Jaw and joint pain and discomfort:
Because the lower jaw is forward, there will be extra pressure on the temporomandibular joint (TMJ). This can lead to jaw pain, headaches, or problems such as clicking and locking of the jaw joint.
Impaired Closing of the Teeth (Malocclusion):
Mandibular prognathism causes class III malocclusion, that is, the upper and lower teeth do not close properly. The lower teeth close in front of the upper teeth. Another term for this condition is reverse bite.
Tooth wear:
Mandibular prognathism-induced malocclusion will result in an abnormal pressure distribution on the teeth. This can cause the teeth to wear faster.
A mouth structure that is open to problems:
When the upper and lower jaws do not fit together, the mouth becomes vulnerable to issues such as gum problems and tooth decay. The jaw may also be vulnerable to trauma.
Speech Disorders:
Misalignment of the jaw and teeth can lead to speech disorders, as it can make it difficult to pronounce certain letters correctly.
Aesthetic Problems:
Positioning the lower jaw forward will result in a symmetry issue within the facial structure. Therefore, patients with this problem may experience aesthetic concerns, potentially leading to a decrease in their self-confidence in society.
How is mandibular prognathism treated?
Pre-treatment investigations:
The first goal of diagnosis and treatment of prognathism is to achieve a healthy skeletal base for healthy occlusion of the teeth and proper posture of the soft tissue. Panoramic radiographs are examined. Problems with discomfort in the temporomandibular joint during chewing and history of psychological disturbance are considered.
Movements of the mandible are noted clinically to determine whether there are abnormalities during closing, opening, lateral, and protruding movements. Facial muscles are examined both during the initial clinical examination and from photographs. Teeth are examined for early contact and wear patterns.
After examining the condition of the teeth, gums, and jawbone, a treatment procedure is determined, taking into account the problems expressed by the patient. One of the following three options for treatment can be applied.
Orthodontic Treatment:
The patient's jaw disorder is mild and not severe. Orthodontic procedures (braces, etc.) can align the jaw and teeth.
Surgery:
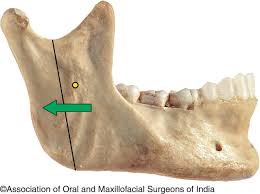
Orthognathic surgery typically takes place in advanced mandibular prognathism. The main purpose of the surgery is to surgically reposition the lower jaw.
If the teeth require overbalancing, orthodontic treatment can be performed before surgery. Teeth usually undergo this treatment, which can last from a few months to a year, with braces or other methods.If minimal balance is required, orthodontic treatment can be performed before surgery.
Mandibular prognathism surgery provides a functionally better jaw closure and aesthetically a more symmetrical facial appearance.
Surgical procedure for mandibular prognathism:

In surgery, also known as orthopedic surgery, the mandible is moved back through a number of surgical procedures. The surgery is performed under general anesthesia. The patient is given oxygen through a nasal tube to give the surgeon unobstructed access to the mouth. Instead of approaching the jaw from the outside, the surgeon makes incisions in the gums to expose the jaw. The bone is then cut and shifted as needed to correct the abnormal protrusion. Bone can also be taken from a different part of the patient's body and added to the jaw if necessary. The jaw is held together and secured with small plates and screws that help to permanently displace the jaw bones and help with a proper bite.
Postoperative Recovery Process
The temporary conditions expected after surgery (pain, swelling, etc.) disappear in a short time, and the patient recovers completely in about nine to 12 months after orthognathic surgery.
Orthodontic treatment can continue for a while after surgery if it's necessary for the jaw position to settle permanently after surgery and for the teeth to fully adapt.
Combined Treatment:
In cases of very severe mandibular prognathism that cannot be corrected by orthodontic treatment or surgery alone, orthodontic treatment and surgical intervention are applied in combination.
Malocclusion:

Malocclusion is a condition in which the upper and lower teeth are not aligned, do not fit together properly and do not close properly.
Causes of Malocclusion:
- Genetic Factors
- Abnormalities in tooth development (early loss of baby teeth in infancy or late eruption of permanent teeth can affect tooth alignment).
- Childhood Habits (Finger sucking, pacifier or bottle use, etc.)
- Tooth grinding
- Tooth loss.
- Poor oral hygiene and tooth decay
- inappropriate crowns, bridges or other dental restorations.
- Mandibular prognathism or maxillary prognathism and TMJ disorders
- Tumors and cysts in the jaw bones or gums
- Orthodontic Problems (teeth not naturally aligned properly, crowded teeth or gaps, etc.)
- Traumas
Symptoms of malocclusion:
The symptoms and severity of malocclusion can vary from person to person.Common symptoms include:
- Cheek biting.
- Difficulty biting or chewing.
- Jaw pain
- Sensitivity of the teeth,
- Whispering or other speech problems.
- Mouth breathing.
- Changes in facial aesthetics.
Types of malocclusion:
Malocclusion is classified according to the jaw structure and the position of the upper and lower teeth.
Class I malocclusion:
The upper teeth meet slightly ahead of the lower teeth.
Class II malocclusion:
The upper teeth meet significantly ahead of the lower teeth. There is an underdeveloped jaw.
Class III malocclusion:
The lower teeth meet well ahead of the upper teeth. There is an overdeveloped jaw structure. It is usually the most difficult type to correct.
Class IV malocclusion:
The upper teeth sit significantly behind the lower teeth.
Class V malocclusion:
The upper teeth sit significantly forward of the lower teeth. There is an overdeveloped jaw.
Class VI malocclusion:
The lower teeth sit significantly behind the upper teeth.
Malocclusion treatment:
The method of treatment depends on whether the patient's condition is mild or severe. One or more of the following treatment types can be applied for malocclusion.
Orthodontic treatment:

Braces:
The most popular treatment method, braces, gradually moves the teeth into the proper position.
Clear aligners:
As an alternative to braces, clear aligners can be used. These align the teeth by moving them slowly.
Fixed and removable appliances:
Fixed or removable appliances are used to change the position of the jaw or to guide its growth, especially in children and adolescents.
Orthognathic Surgery:
Orthognathic surgery can be performed when orthodontic treatment alone is not sufficient, especially if there is a severe misalignment of the jaw bones. Orthodontic treatment aligns the teeth after repositioning the jawbone through surgery.
Tooth Extraction
It typically occurs in conjunction with orthodontic treatment. If the crowding of teeth has led to malocclusion, the extraction of some teeth may be necessary. This creates enough space for the teeth and allows for the proper positioning of the remaining teeth.
Restorative procedures:
Veneers, crowns, implants, etc. can be applied to repair missing or damaged teeth.
Duration of malocclusion treatment:
The duration of treatment depends on the general health of the patient, the severity of the dental malocclusion, and the condition of the jawbone, teeth, and gums. In some severe cases, it may take up to two years.
What treatment was given to Michael Van Gerwen?
As can be seen from Michael Van Gerwen's statements to the press, a combined treatment was applied. First, the protruding mandible was surgically repositioned to its normal position, and then orthodontic treatment was started. Michael Van Gerwen will wear the braces for malocclusion for a while longer, and the treatment will end once his teeth are fully aligned.
FAQ:
Is prognathism more common in men or women?
Prognathism affects both men and women but is slightly more common in men.
Does the mandible prognathism heal completely?
Surgical treatment also results in a significant aesthetic improvement. Facial features become softer, slimmer, and more harmonious.
What happens if mandibular prognathism is not treated?
If mandibular prognathism is not treated, the following problems will ocur:
- Difficulty in daily functions and reduced quality of life
- Chewing and digestion problems
- Jaw and jaw joint problems
- Tooth wear and caries
- Teeth grinding and clenching.
- Speech disorders
- Mouth breathing and respiratory problems
- Sleep apnea
- Aesthetic concerns and lack of self-confidence
Should I undergo another surgery to remove the plates and screws inserted into my jaw during the prosthesis procedure?
Prognathism surgery typically inserts plates and screws to fix the jaw bones in their new position, leaving these materials in the jawbone permanently. Biocompatible materials, typically titanium, form these plates and screws, which the body tolerates well, eliminating the need for their removal during a subsequent surgery. In the majority of patients, the plates and screws adapt to the jawbone and do not cause any lifelong problems.
What should be considered after prognathism surgery?
Swelling and bruising following the surgery is expected. There is no need to worry. It will pass in a short time. You can use the painkillers prescribed by your doctor to reduce the pain. You can apply cold compresses to reduce swelling. In addition to these, you will need to pay attention to the following points:
- Soft or liquid foods should be taken
- Avoid hot food and drinks
- Pay attention to oral hygiene
- You should rest for a few days after surgery.
- Excessive jaw movements should be avoided
- Avoid smoking and alcohol consumption
- Keep the follow-up appointments given by the doctor.
What happens if malocclusion is not treated?
Untreated malocclusion can lead to conditions such as
- Gum recession.
- Injury to the gums.
- Jaw pain.
- Malnutrition due to chewing problems.
- Sleep apnea or other sleep disorders.
- Tooth erosion.
Note:This article is intended to provide general information about mandibular prognathism and related treatments, based on the experience of Michael van Gerwen. Information about Michael van Gerwen is taken from open sources and may not include exact or up-to-date details. This content is for informational purposes only and is not a substitute for professional medical or dental advice. It is important to consult a qualified dentist who can assess your individual needs and determine the most appropriate treatment plan. Individual results and needs may vary.
